Lacrimal Procedures
DACRYOCYSTORHINOSTOMY (dcr) FOR TEAR DUCT OBSTRUCTION
How do tears normally function?
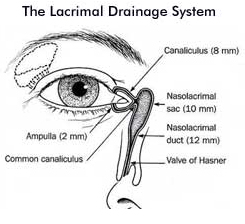
Tears are made primarily by the lacrimal gland, which is anatomically located under the outer one-third of the upper eyelid. With each blink, the eyelid spreads tears over the surface of the eye and pumps excess tears towards ducts in both the upper and lower eyelids. These ducts then drain the tears into the nose via the nasolacrimal duct.
What causes tearing disorders?
 |
 |
Epiphora, or watery eyes, can be congenital or acquired.
Congenital lacrimal duct obstruction (in either one or both eyes) occurs in approximately 20% of infants. This percentage is even higher in premature babies. In most infants, the obstruction is caused by a membrane at the base of the tear duct just before the duct enters the nose.
Acquired (adult-onset) nasolacrimal duct obstruction can be caused by several factors. Involutional (age-related) nasolacrimal duct obstruction is the most common cause. Other causes include trauma, sinus disease, nasal polyps, tumour or infection.
Read More…
What are the symptoms?
Obstruction of the tear duct will cause epiphora (watering of the eye) because the tears cannot drain properly. Symptoms of a blocked tear duct include eyelashes that are stuck together by mucous or an accumulation of tears in one or both eyes. The tears trapped within the duct may become infected causing a painful swelling in the inner corner of the eyelid. This condition is called ‘dacryocystitis’ (an inflammation of the lacrimal sac), which may also be caused by a stone in the lacrimal sac.
How is Nasolacrimal Duct Obstruction diagnosed?
Diagnosis of acquired nasolacrimal duct obstruction is required with one or more in-office tests by Dr Martin. This may include a dye disappearance test, whereby fluoroscein dye is placed on the eye surface, and the disappearance between the two eyes compared. A second test for obstruction of the nasolacrimal duct might include irrigation of the tear drainage pathways. This non-painful test is conducted by placing a small, blunt irrigating syringe inside the opening of the tear duct, and irrigating fluid (water or saline) through the tear drainage system. If the nasolacrimal duct is found to be relatively or completely obstructed, a DCR procedure is often indicated.
What is the treatment for watery eye?
Initial treatment of infants with congenital nasolacrimal duct obstruction involves massaging the area over the affected tear sac (located under the skin between the eye and nose) to force the tears and mucous from the sac, hopefully pushing open the membrane causing the obstruction. This is to be done properly and frequently, and is generally continued until the tearing resolves. Dr Martin may also prescribe antibiotic ointments or drops.
In 80% of infants the blockage resolves by 6 months of age. If it still persists beyond 6 months, it may be necessary to open the tear duct by probing and irrigation. These are most commonly performed between 6 months and one year of age, and may be conducted in the rooms or in hospital with the child under a brief monitored anaesthetic. Unfortunately, blockages may recur in spite of probings. If the tearing persists, then a tiny silicone tube may be placed down the duct to keep the tear drainage system open. This usually remains in place for 3-12 months to prevent the obstruction from recurring.
In adults with acquired nasolacrimal duct obstruction, a dacryocystorhinostomy (DCR) procedure is performed if indicated.
What is DCR surgery?
A DCR is the surgical creation of an opening between the lacrimal sac and the nasal cavity to form a new drainage channel for tears.
In the DCR procedure, the tear drainage pathways are reconnected to the inside of the nose. A small incision is made at the side of the nose, and the lacrimal sac is located, incised and then connected to the nasal mucosa creating a new tear drainage pathway. A tiny plastic tube (Jones tube) is then placed in the newly created tear drainage pathway to prevent scarring of the tear drainage duct, which might otherwise result in failure of the surgery.
What can I expect after DCR surgery?
Most patients should expect immediate resolution of their watery eye, however, in some patients the tearing may persist for some time. This is normal, however, you must inform Dr Martin of this.
After surgery there is generally very little pain associated with the operation, although there is some soreness. Minor bruising and swelling may be expected. This will gradually resolve and complete healing may take up to 6 weeks. If sutures are present they will be removed 5-7 days post-operatively. Dr Martin will prescribe antibiotic ointment that is to be used on the wound.
You should avoid hot food and drinks for 24 hours post-operatively. No aspirin or aspirin-based medications should be taken for pain for about one week following the surgery as there will be a tendency for a nosebleed. You should also refrain from blowing your nose aggressively.
Most patients can return to work approximately 1 week after the surgery.
If a tube is used this is usually removed in the office with little discomfort, approximately 3-6 months following the surgery.